Independent Claims Reviews: A Fiduciary Imperative
- Dec 12, 2025
- 2 min read

Introduction
For many plan sponsors, the word “audit” suggests penalties or after-the-fact corrections. In reality, independent claims reviews are about prevention, transparency, and protecting plan assets — not punishment.
Why Reviews Matter
ERISA and the Consolidated Appropriations Act (CAA) require fiduciaries to act prudently and solely in the interest of participants. That means monitoring service providers to ensure claims are processed correctly, fees are reasonable, and conflicts of interest don’t drain plan assets.
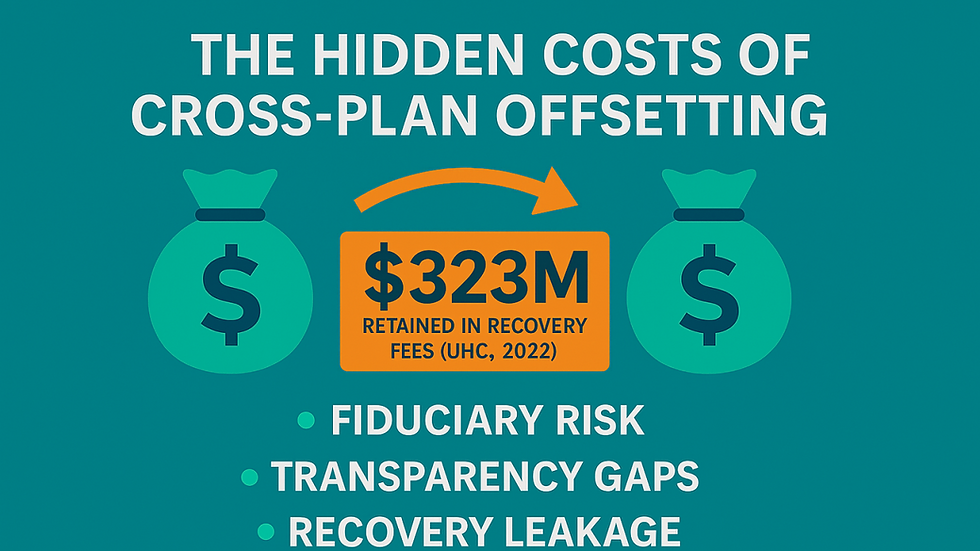
The Risks of Relying Solely on Carriers/TPAs
Carriers and TPAs profit when claims move quickly, even if errors slip through. Remember, it’s not their money they’re spending, it’s yours.
Post-pay “savings” programs reward inefficiency rather than prevent it.
Without independent validation, plan sponsors cannot confirm accuracy or fiduciary compliance.
Independent Reviews = Fiduciary Compliance
Validate claim accuracy.
Detect overpayments and ensure recoveries return to the plan.
Align vendor practices with fiduciary duties.
Document prudence for regulators and participants.
Safeguard against conflicts of interest.
From Audit to Oversight
Instead of treating these as “audits,” plan sponsors should view them as:
Oversight reviews – confirming fiduciary responsibility.
Validation checks – ensuring accuracy of claims and vendor performance.
Transparency reviews – protecting participants through full data access.
More Than Cost Containment
While catching billing errors, payment mistakes and waste is valuable, the fiduciary purpose of claims reviews runs deeper:
Protecting plan assets – every dollar lost to errors is participant money.
Monitoring service providers – TPAs, PBMs, and networks must be held accountable.
Validating accuracy guarantees – “99% accuracy” claims often crumble under scrutiny.
Documenting prudence – courts emphasize process; reviews demonstrate active oversight.
Fiduciary Checklist for Claims Reviews
Employers should ensure reviews address:
Payment accuracy – Are claims paid correctly the first time?
Recovery oversight – Do funds flow back to the plan?
Fee transparency – Are administrative charges fully disclosed?
Data access – Does the employer control claims data?
Documentation – Are results and corrective actions recorded?
The Fiduciary Imperative
The Department of Labor has made clear: fiduciary responsibility cannot be delegated away. Employers who fail to conduct independent reviews risk financial leakage — and fiduciary liability.
At ClaimInformatics, we help employers:
Conduct independent reviews for accuracy and compliance.
Identify systemic errors that drive costs.
Document oversight to protect fiduciaries and participants.
Conclusion
Fiduciary compliance requires more than trust, it requires verification. Independent claims reviews safeguard plan assets, participants, and demonstrate the prudence while monitoring service provides, all what regulators and courts expect.
Get your free e-book on Fudiciary Guidelines for Self-Funded Plans.


Comments