Protect Yourself and Your Self-Funded
The Critical Need for Fiduciary Compliance
Navigating the complexities of self-funded healthcare plans is no small task. With mounting regulatory pressure, rising claim errors, and an increase in lawsuits targeting fiduciaries, ensuring financial integrity and compliance has never been more critical. ClaimInformatics delivers comprehensive solutions that go beyond traditional claims review—providing proactive oversight, forensic insights, and continuous protection. Partner with us to safeguard your plan’s financial health, mitigate legal exposure, and fulfill your obligations under ERISA and the CAA.
The Current System Is Working Against You
Networks profit by fixing their own mistakes through post-payment review programs, essentially getting paid to correct errors they made.
Revenue optimization happens at the expense of the plan sponsor, with providers benefiting while the costs are passed on to you.
It’s not their money; networks and TPAs benefit from errors, while most absolve themselves of fiduciary responsibility.
Auto-adjudication prioritizes speed over accuracy, leading to unaddressed mistakes and overpayments.
Networks collect fees regardless of outcomes, whether claims are valid or erroneous, further incentivizing inaccuracy.
.png)
Opacity is not your friend. The only way to identify these issues and protect yourself and your plan from fiduciary risk is to obtain your data, monitor your service providers, ensure there are no conflicts of interest, be prudent, ensure fees are reasonable, and ensure plan documents are being followed. How can a fiduciary meet these obligations without reviewing their data?
Fraud, Waste and Abuse – Typical Findings Happening In Your Plan Today
$114,672
Upcoding Fraud
$48,000
Hidden Fees
$38,000
Billing Inconsistency
FOCUS by ClaimInformatics
TM
Fiduciary Oversight, Compliance, & Utilization Safeguard
.png)
-
One to three-year historical claims analysis evaluating 100% of claims
-
Flags pricing errors, abuse, and systemic payment failures
-
Valuable diagnostic tool for uncovering past inefficiencies and assessing fiduciary oversight risks
-
Ensures compliance with ERISA,
CAA, as well as plan documents -
Identifies financial leakage and overpayment at the source
-
Creates a defensible audit trail and reinforces prudent plan oversight
-
Proactive, fiduciary-focused solution monitors claims monthly, ensuring compliance and early issue detection
-
Recovers identified overpayments
-
Fulfills fiduciary obligations by
restoring plan assets -
Included with PAIR and OM, client receives 50% of recovered funds
ClaimInformatics is the only comprehensive solution that delivers fiduciary protection while transforming raw claims data into strategic insights. Our platform ensures transparency, reduces liability, and maintains compliance—while driving measurable cost savings. By identifying overpayments, errors, and patterns of excess spend, we provide concrete evidence of value through validated financial recovery and actionable documentation. Our SOC 2-certified, HIPAA-compliant service delivers enterprise-grade oversight typically reserved for the largest organizations—now accessible to self-funded plans of all sizes.
.png)
.png)
Driving Fiduciary Compliance & Oversight
At ClaimInformatics, we help self-funded plans fulfill their fiduciary responsibilities with precision, transparency, and confidence. Our range of services helps identify, recover, and prevent improper payments at various stages of the claims process. ClaimInformatics transforms your organization's risk profile using independent oversight and advanced technology. We help you stay ahead in a complex ecosystem, offering integrated protection and navigating regulatory challenges to give you peace of mind and keep more money in your pocket.
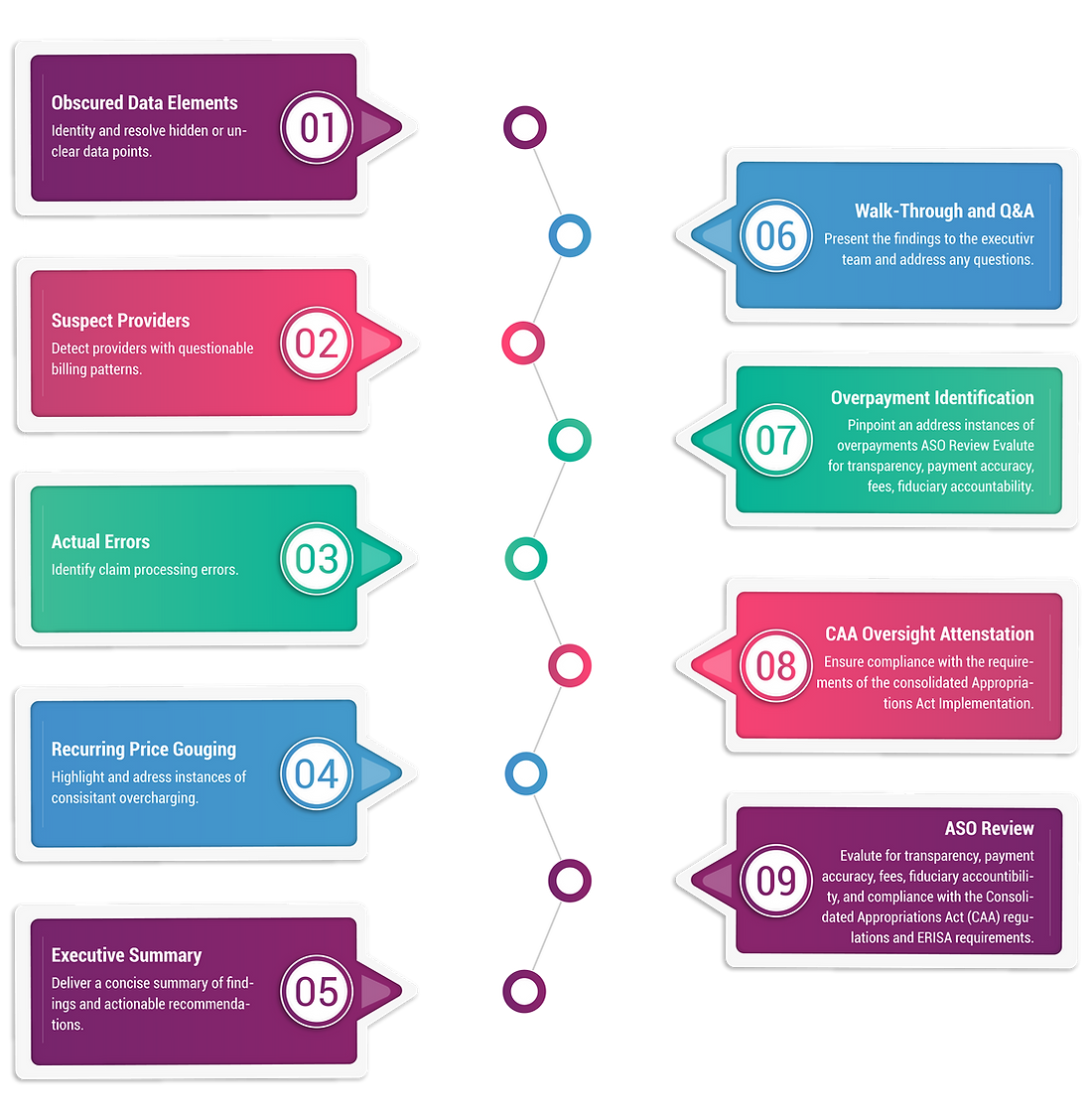
Your Path Forward To Fiduciary Oversight Excellence
.png)
PAIR
Plan Accountability & Integrity Review
The PAIR report delivers a comprehensive one to three-year analysis of paid claims, uncovering improper payments to support fiduciary compliance for self-funded plans.
Reviews 100% of claims against millions of industry-standard rule sets
Over 850 proprietary algorithms/edits, including our exclusive Episode of Care™ logic
Combines advanced automation with expert analysis
Equips plans with actionable insights to recover improper payments
Helps meet fiduciary obligations confidently

PAIR serves as a valuable diagnostic tool for uncovering past inefficiencies and assessing overall fiduciary risks.
Key Deliverables
On-Going Monitoring
At ClaimInformatics, we understand the critical responsibility that benefits managers and fiduciaries of self-funded healthcare plans face. Our On-Going Monitoring (OM) solution is a proactive, fiduciary-focused solution that continuously monitors claims on a monthly basis — now enhanced with real-time analytics and an intuitive dashboard. This near real-time oversight not only ensures ongoing compliance and early detection of emerging issues, but also gives you complete transparency into how your plan is spending money.

Our platform delivers actionable insights at your fingertips, allowing you to:
Identify high-cost members, suspect providers, and top procedures
Detect overpayments and errors before they accumulate
Drive recoveries and ensure accurate claim payments
Share findings with the network or TPA for resolution
Manage or support the recovery process
Safeguard compliance and accountability
Complete Transparency
Our platform analyzes 100% of claims data, with dynamic dashboards that give you a clear, real-time view of where every dollar is going. From high-cost claimants to questionable provider patterns and most common procedures, nothing falls through the cracks.
Reduced Fiduciary Risk
Early detection of improper payments, suspect billing practices, and deviations from plan documents helps prevent costly errors—protecting both personal and organizational fiduciary responsibilities.
Actionable Intelligence
Our dashboard transforms complex claims data into clear, actionable insights. Monthly monitoring and real-time analytics work together to provide continuous compliance recommendations and help you make data-driven decisions.
Quantifiable Value
Demonstrate your effectiveness with clear, measurable savings that protect plan assets and reinforce your fiduciary role. ClaimInformatics empowers you with continuous, data-driven oversight—analyzing 100% of your healthcare claims to uncover billing anomalies, outlier provider behaviors, and compliance gaps that would otherwise go unnoticed.
Our platform provides plan sponsors with real-time insights into service provider performance, benefit utilization trends, and adherence to contractual terms—enabling proactive decision-making and reducing reliance on retrospective audits. With average annual findings of $82.37 per employee (actual results may vary), our approach delivers verifiable financial value while enhancing fiduciary governance.
Learn how our FOCUS solutions support continuous monitoring, informed oversight,
and strategic accountability across all stakeholders in your health plan ecosystem.
.png)