Navigating Healthcare Fraud Risks and the BUCA Rebellion: A Guide for Self-Funded Plans
- Oct 19, 2025
- 3 min read
In today's rapidly evolving healthcare landscape, staying ahead of fraud risks and optimizing costs are top priorities for employers managing self-funded health plans. At ClaimInformatics, we deliver comprehensive payment integrity solutions that not only detect overpayments but also provide powerful pre-payment interventions to stop errors before they occur. Our approach ensures accurate coding, prevents improper claims, and supports ongoing compliance.
We will delve into the recent insights from the U.S. Department of Health and Human Services' Office of Inspector General (OIG) regarding the government's enforcement priorities under the False Claims Act (FCA). Additionally, we will discuss the growing trend of moving away from traditional "BUCA" carriers towards self-funded models. These models provide employers with greater transparency, fiduciary alignment, and control. In this environment, integrating robust solutions like Claiminformatics can maximize value.

Understanding the OIG's Fraud Risk Spectrum
The OIG's Fraud Risk Spectrum is a key framework for addressing healthcare fraud, primarily through the use of the FCA. Most cases are settled without admission of liability, and the OIG categorizes outcomes based on the perceived risk to federal programs, such as Medicare and Medicaid. This spectrum ranges from high-risk exclusions (banning entities from federal programs) to low-risk self-disclosures, where voluntary reporting often leads to leniency.
Recent data shows a consistent trend: In FY 2025 (Q1-Q4), there were 9 exclusions, 1 heightened scrutiny case, 22 Corporate Integrity Agreements (CIAs), 199 "no further action" resolutions, and 7 self-disclosures. This pattern highlights the OIG's preference for proportional responses, rewarding cooperation, and self-audits. For self-funded plans, this underscores the importance of proactive claims reviews to avoid similar scrutiny in commercial settings.
For more details, check out the OIG's official page: Fraud Risk and Heightened Scrutiny.
Heightened Scrutiny: A Warning Sign for Providers
Heightened scrutiny is reserved for entities that settle FCA cases but refuse to provide CIAs, leading to public listing on the OIG's website. As of October 2025, there are nine such cases, including those involving providers in Indiana, Colorado, and New York, often linked to improper billing. This public "watch list" serves as a deterrent and a tool for payers to flag high-risk providers.
At ClaimInformatics, we recommend integrating this list into your claims processing. Our reviews can spot anomalies in coding (e.g., CPT or HCPCS errors) from these entities, potentially recovering 5-10% in overpayments.
Explore the full list here: Browse CIAs - Heightened Scrutiny.
What Are BUCA Plans?
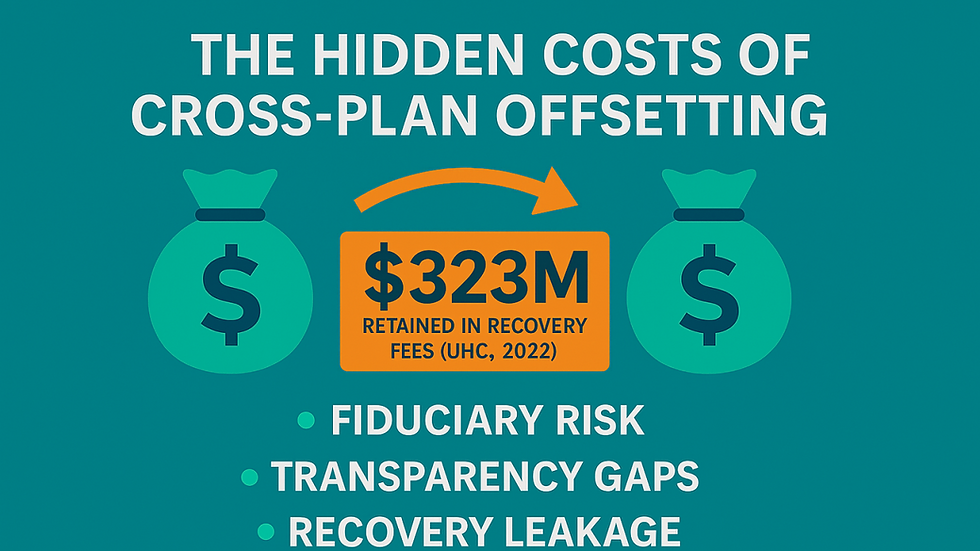
"BUCA" is industry shorthand for the four major health insurance carriers that have dominated the market for over 150 years: Blue Cross Blue Shield, UnitedHealthcare, Cigna, and Aetna. These fully insured plans offer broad networks and handle all administrative tasks, but they often come up with rising premiums (10+% annually), limited customization options, and opaque cost structures.
While convenient, BUCA plans to shift financial risk to the carrier, leaving employers with little insight into claims data. This can mask inefficiencies, such as overbilling, which ties back to the fraud risks outlined by the OIG.
The Great Shift to Self-Funded Plans
Employers are increasingly opting for self-funded alternatives to BUCA, driven by the promise of savings exceeding 20%, full data transparency, and flexibility under ERISA regulations. In 2025, this "exodus" from fully insured plans is accelerating, with innovations such as level-funded options and group captives making self-funding more accessible even for mid-sized groups.
Self-funded plans allow direct provider contracts, unbundled services (e.g., independent pharmacy benefit managers), and proactive fraud detection, aligning perfectly with OIG's emphasis on self-disclosure and integrity. Amid rising costs, these plans are evolving from mere cost-cutters to value-builders, incorporating wellness incentives and advanced analytics. Employers gain access to raw claims data, enabling tools like ClaimInformatics to audit errors and recover funds efficiently.
Why Payment Integrity Matters in This Transition
Whether you're monitoring OIG-listed providers or transitioning from BUCA, payment integrity is your safeguard. At ClaimInformatics, our solutions for self-funded plans use AI to ensure accurate payments, detect fraud early, and promote compliance—helping you avoid the pitfalls seen in FCA settlements.
Ready to enhance the integrity of your plan? Contact us at ClaimInformatics for a free consultation and start saving today.


Comments