Hidden Fees in Self-Funded Health Plans: The Next 401(k) Crisis?
- Oct 24, 2025
- 3 min read
Introduction
When 401(k) plans first came under fire for excessive fees and opaque vendor practices, employers faced a wave of lawsuits that reshaped retirement governance. Today, a similar story is unfolding in healthcare: hidden fees in self-funded plans are becoming the next fiduciary crisis.

The key phrase to remember is "fiduciary self-funded plans with hidden fees." Under ERISA and the Consolidated Appropriations Act (CAA 2021), employers must not only provide benefits, but also demonstrate that fees are transparent, reasonable, and in the best interests of the plan and its members.
The 401(k) Fee Parallel
401(k) litigation taught us that “small” hidden fees can add up to millions in lost participant value. Cases like Tussey v. ABB and Tibble v. Edison made it clear that fiduciaries must continuously monitor costs, not just at contract signing.

That same fiduciary duty now extends to health plans: every dollar lost to opaque broker/TPA payments, spread pricing, or undisclosed rebates comes directly out of members’ pockets.
Where Hidden Fees Lurk in Self-Funded Plans
Employers may not realize just how many hidden charges can erode plan value:
Broker & Consultant Compensation: Undisclosed overrides, bonuses, or indirect payments.
Third-Party Administrators (TPAs): Marked-up network access fees or unchallenged administrative charges.
Pharmacy Benefit Managers (PBMs): Retained rebates, spread pricing between wholesale and billed drug costs, and opaque formulary management.
Stop-Loss Contracts: Complex pricing structures that hide true margins.
Without access to claims data, employers often have no visibility into these hidden costs.
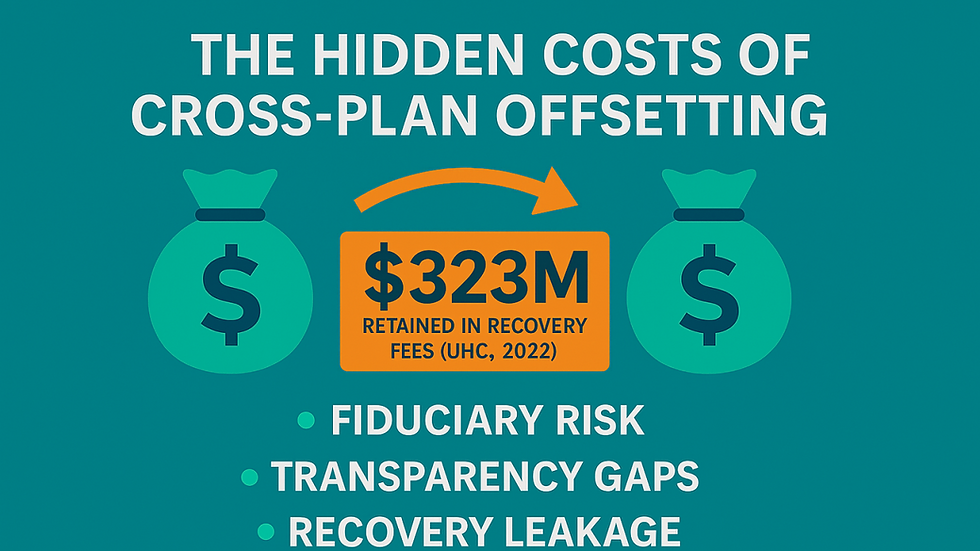
The Fiduciary Risk Is Real
Recent lawsuits have already targeted employers for failure to control hidden fees. Courts are applying the same fiduciary standards used in 401(k) fee litigation to health plans. Employers who cannot demonstrate prudent oversight of costs risk:
ERISA fiduciary breach claims
Employee Benefits Security Administration (DOL’s ERISA enforcement arm)
Reputational damage and employee distrust
What Employers Must Do to Stay Compliant
To protect against fiduciary risk, employers must bring the 401(k)-fee playbook into healthcare:
Demand Fee Transparency: Require full disclosure of broker, consultant, TPA, and PBM compensation—direct and indirect—a CAA requirement.
Secure Data Access & Audit Rights: Ensure contracts allow independent audits and unrestricted access to claims data.
Benchmark Vendor Costs: Compare fees against independent data and market standards every 12–24 months.
Document Oversight Processes: Record all committee decisions, vendor negotiations, and compliance steps.
Engage a Prudent Expert: If your team lacks internal expertise, ERISA allows fiduciaries to delegate oversight — but not responsibility — to qualified advisors like Fiduciary in a Box.
Conclusion
Hidden fees were once the silent drain on 401(k) plans until fiduciary litigation forced a reckoning. Self-funded health plans are now entering the same era of scrutiny. Employers who fail to demand transparency may soon face the next wave of fee lawsuits.
By proactively uncovering hidden costs, benchmarking vendors, and documenting fiduciary processes, employers can turn compliance into a competitive advantage — protecting both employees and the organization.
✅ Call to Action
ClaimInformatics helps employers uncover hidden fees, enforce transparency, and build defensible fiduciary processes. Fill out this form and get your free guide to Fiduciary Oversight for Self-Funded Health Plans and safeguard your plan against the next 401(k)-style crisis.


Comments