Claim Audit vs. Claim Review: Why Fiduciaries Must Know the Difference For ERISA and CAA Compliance
- Oct 21, 2025
- 2 min read

Introduction
In employee health benefit plans, “claim audit” and “claim review” are often used interchangeably. But the two terms mean very different things — and the difference matters deeply for fiduciaries.
Under ERISA, fiduciaries are not only tasked with ensuring compliance but also with safeguarding plan assets, monitoring service providers, and acting solely in the interest of participants. Understanding where an audit ends and a review begins is essential to fulfilling those duties.
🔍 What Is a Claim Audit?
A claim audit is a limited right outlined in the Administrative Services Only (ASO) agreement with a third-party administrator (TPA) or carrier.
Key traits of audits
Restricted Data Access – Employers rarely gain full claim-level data; only summaries or redacted reports are provided.
Sample-based – A narrow slice of claims is reviewed, not the entire population of claims.
Non-extrapolative – Errors found in the sample don’t necessarily apply across all claims.
Carrier-controlled – Bound by ASO rules and audit protocols.
No Fiduciary Accountability – The carrier disclaims fiduciary responsibility, shifting ultimate accountability back to the plan sponsor.
👉 While audits can highlight issues, they provide only a restricted view of plan operations — and may create a false sense of security for fiduciaries.

✅ What Is a Claim Review?
A claim review, by contrast, is rooted in fiduciary responsibility under ERISA. It is broader, continuous, and independent of ASO contract terms.
Key traits of reviews:
Comprehensive – Covers all claims, not just a sample.
Fiduciary-driven – Ensures assets are used prudently and solely for participant benefit.
Plan-focused – Ensures benefits are paid strictly according to governing plan documents.
Ongoing oversight – Identifies patterns, prevents waste, and detects abuse in real time.
Actionable outcomes – Provides data for corrections, recoveries, and plan improvements, enabling fiduciaries to remedy breaches when issues arise.
Legal obligation – Fiduciaries cannot outsource or ignore this responsibility.
👉 Reviews are not optional. They are the processes fiduciaries must undertake to meet legal and ethical standards.
⚖️ Why the Difference Matters For ERISA and CAA Compliance
The distinction can be summarized:
Audit = What the carrier allows.
Review = What ERISA requires.
Audits are carrier-controlled checkpoints with a narrow scope. Reviews demonstrate proactive fiduciary oversight, providing transparency, accountability, and protection for plan participants.
Without reviews, fiduciaries risk:
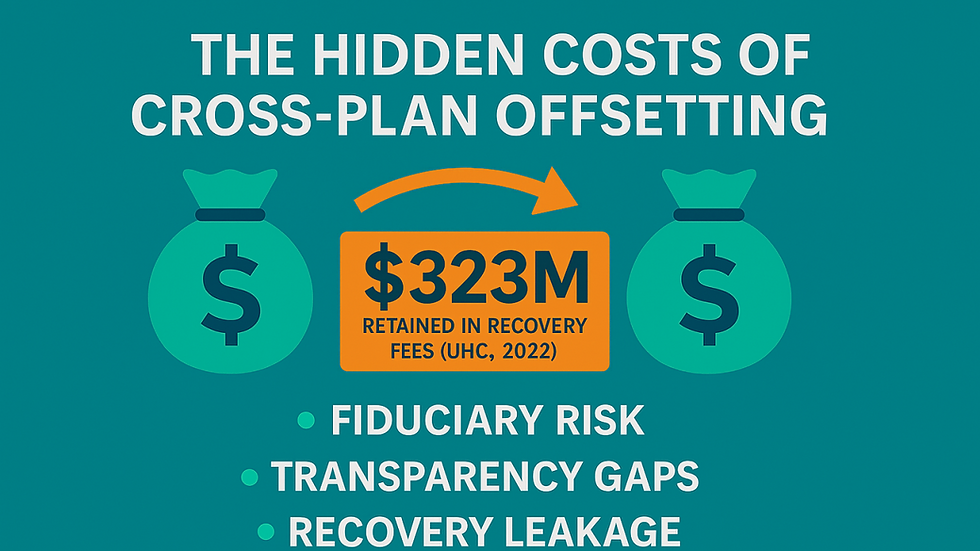
Financial leakage from undetected errors.
Hidden vendor conflicts of interest.
Potential liability for failing to meet ERISA’s prudence standards.
📌 The Fiduciary Takeaway
Claim audits and claim reviews are not interchangeable. Audits may be useful for compliance snapshots, but only reviews fulfill fiduciary obligations.
A prudent fiduciary will:
Conduct regular claim reviews for independent oversight.
Verify service provider accuracy.
Ensure plan provisions are enforced.
Protect participant assets with documented processes.
At ClaimInformatics, we help fiduciaries move beyond carrier-controlled audits to true oversight, empowering them with transparency, validation, and confidence in their fiduciary role.


Comments