The Tide Has Turned: No More Excuses on Data Access and Oversight
- Nov 26, 2025
- 3 min read

Major networks are finally shifting on data sharing — the excuses are gone. It is the employer’s fiduciary responsibility to demand access. If a carrier or vendor refuses, and the pattern continues, you must replace them because their obstruction causes you to breach your fiduciary obligations.
Introduction
For years, self-funded employers were denied full access to claims data, with networks and vendors dismissing it as proprietary and confidential information they deemed impossible or impractical to share. Those excuses no longer hold. The tide has turned, and major networks are loosening their grip on the data employers rightfully own.
Access is your right. If you’re not demanding your data, analyzing it, and acting on it, you are falling short of your fiduciary duty.

The Shift in Network Data Practices
Networks have long walled off claims data under the guise of 'confidentiality' or 'contractual restrictions.' But mounting legal, regulatory, and market pressures are dismantling those barriers. The Consolidated Appropriations Act (CAA) now prohibits gag clauses and guarantees plan sponsors access to their data, and networks are complying not by choice, but by obligation and client demand.
For fiduciaries, the mandate is clear: vendor pushback is no longer acceptable. Employers must demand data access, ensure it is usable, and act on it to fulfill their fiduciary duty.
Why Data Access Is Non-Negotiable
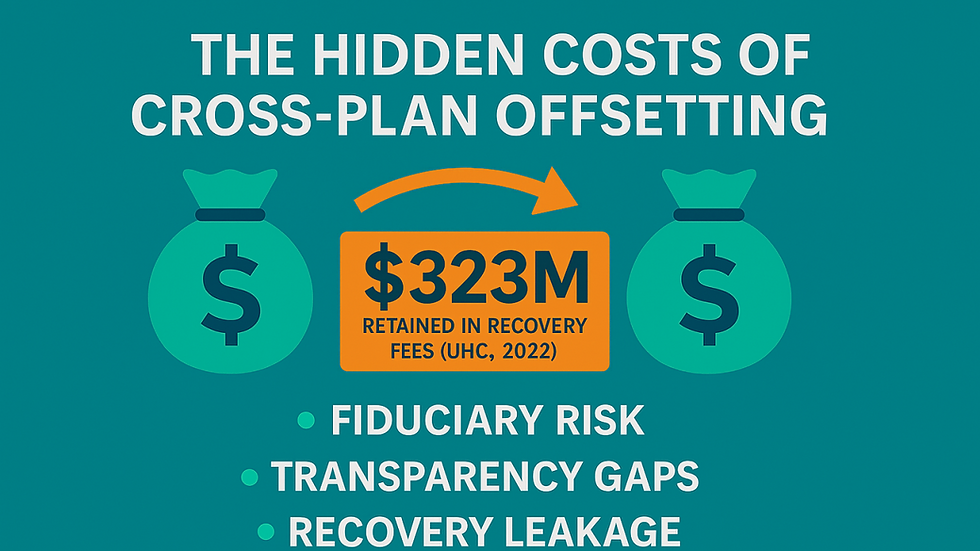
Every dollar spent on healthcare claims comes directly from plan assets. Without data, employers are blind to waste, overbilling, and hidden revenue streams benefiting intermediaries. The absence of oversight isn’t just costly, it’s a fiduciary breach.
Access to claims data unlocks your ability to:
Identify billing and payment errors.
Evaluate vendor performance with objective evidence.
Benchmark costs against independent standards.
Prove compliance with ERISA fiduciary requirements.
In short, data access isn’t a nice-to-have. It’s the foundation of fiduciary accountability and is a core administrative function of the plan.
What Employers Must Require in RFPs
As data access becomes the norm, employers need to bake these requirements into every RFP and vendor contract:
Unrestricted Claims Data Access: Require full, timely feeds of medical and pharmacy claims.
Oversight Rights: Maintain the authority to perform independent claim reviews as needed, balancing administrative functions with fiduciary obligations.
Review Rights: Secure the contractual ability to examine claims activity to protect plan assets and participants independently.
Transparency on Vendor Compensation: Demand disclosure of all direct and indirect payments.
Independent Pre-Pay Claim Review: Move beyond “pay now, chase later” by requiring third-party review of claims before they’re paid.
RFPs set the tone for accountability and fiduciary compliance. If these protections aren’t explicitly required, you’re leaving money and compliance on the table.
Turning Data into Action
Having data isn’t enough. Plan sponsors must put it to work:
Conduct ongoing monitoring to detect patterns of overpayment.
Implement corrective action when vendors fall short.
Document fiduciary oversight to safeguard against regulatory or legal scrutiny.
An independent pre-pay claim review sets the highest standard of protection by verifying charges before plan funds are released. But when pre-pay isn’t available, post-pay reviews remain essential. They identify errors, enforce accountability, and ensure recoveries are returned to the plan, protecting employees’ health dollars with integrity.
Conclusion
The era of excuses is over. Networks can no longer shield claims data behind “confidentiality” or restrictive contracts. Employers not only have the right to access this data, but they also have the fiduciary duty to demand it, use it, and act on it.
Failing to do so doesn’t just leave money on the table; it exposes fiduciaries to regulatory, legal, and financial risk. Under ERISA, inaction is a breach. By requiring transparency, embedding oversight in every RFP, and leveraging independent claim review. Ideally, pre-pay, but post-pay when necessary — employers transform compliance into protection for plan assets and participants.
✅ Call to Action
ClaimInformatics equips employers with the tools to demand data, enforce accountability, and implement independent claim reviews that protect both participants and fiduciaries. Please reach out to us today to turn oversight into measurable savings and defensible compliance. You can learn more at claiminformatics.com.


Comments