Health Plan Oversight: The Role of Benefits Committees and Fiduciary Duty
- Dec 12, 2025
- 2 min read

In retirement plans, investment committees are a well-established governance structure. They monitor vendors and fees, benchmark performance, and document fiduciary decisions. Increasingly, regulators and courts expect benefits committees to play a similar role in healthcare.
Under ERISA, fiduciaries must act prudently, solely in the interest of plan participants, and ensure plan assets are used appropriately. For self-funded health plans, that duty extends beyond writing checks — it requires active oversight of costs, vendors, and compliance.
🏛 Why Benefits Committees Matter
Parallels to 401(k) Oversight – Just as investment committees review fund performance, benefits committees must review TPA contracts, pharmacy benefit manager (PBM) arrangements, and hospital charges.
Accountability – Fiduciaries cannot delegate responsibility to TPAs or carriers; ultimate liability rests with the employer’s plan fiduciaries.
Governance Structure – A benefits committee formalizes monitoring, sets meeting schedules, and documents prudent processes.
✅ A Fiduciary Checklist for Benefits Committees
1. Review Fees and Contracts
Scrutinize TPA, PBM, and network contracts for hidden fees or revenue-sharing.
Benchmark costs against industry norms and demand transparency.
2. Monitor Claims and Payment Accuracy
Ensure independent reviews are conducted regularly - don’t rely solely on your TPA or Network reporting.
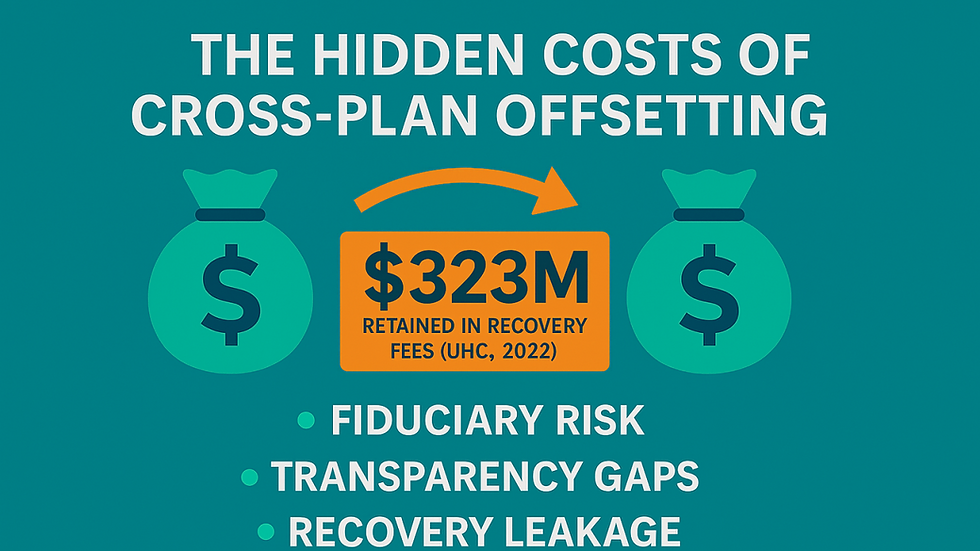
Confirm recoveries are returned to the plan, not retained by vendors.
3. Demand Data Access
Full access to raw claims and recovery data is essential for oversight.
Gag clauses or reporting limitations are not only illegal, they undermine oversight.
4. Document Oversight
Keep minutes of fiduciary decisions and vendor reviews.
Retain audit reports and benchmarking as proof of prudence.
5. Address Conflicts of Interest
Require disclosure of financial incentives and ownership ties.
Ensure all decisions put plan participants first.
🔒 The Fiduciary Imperative
Much like 401(k) governance, health plan oversight must be structured, documented, and member-focused. Plan Sponsors who establish benefits committees demonstrate prudence and strengthen their compliance defense.
At ClaimInformatics, we partner with benefits committees to:
Review Contracts – Uncover hidden fees and conflicts.
Review Claims – Validate accuracy, ensure recoveries return to the plan.
Demand Data – Full access to raw claims and recovery reporting.
Document Oversight – Keep audit-ready records of decisions.
Bottom line: Strong benefits committees = stronger fiduciary protection and measurable cost savings for the plan and its participants.


Comments