FOCUS™ on Fiduciary Compliance: Strengthening ASO Agreements and SPD Protections
- Sep 25, 2025
- 2 min read
Introduction
Self-funded health plans face a growing set of fiduciary challenges, including restricted access to claims data, hidden fees, and conflicts of interest within TPA processes. These challenges can undermine ERISA’s prudent expert standard and compromise the protections outlined in your Summary Plan Description (SPD).

At ClaimInformatics, our FOCUS™ platform (Fiduciary Oversight, Compliance, and Utilization Safeguard)—powered by PAIR™ technology, Ongoing Monitoring, Pre-Pay Payment integrity and Recovery Services, and advanced analytics helps plan fiduciaries safeguard participant assets, enforce SPD protections, and achieve compliance with ERISA and the Consolidated Appropriations Act (CAA).
Fiduciary Compliance Standard
Under ERISA, fiduciaries are required to act with loyalty, prudence, and full oversight. This means:
Protecting plan assets from overpayment and conflicts of interest.
Ensuring transparency in fees and claims data.
Monitoring TPAs with the skill and diligence of a prudent expert.
Where ASO Agreements Fall Short
Administrative Services Only (ASO) agreements often embed risks that erode fiduciary responsibility, including:
Data Restrictions – TPAs delaying or overcharging for access to claims data.
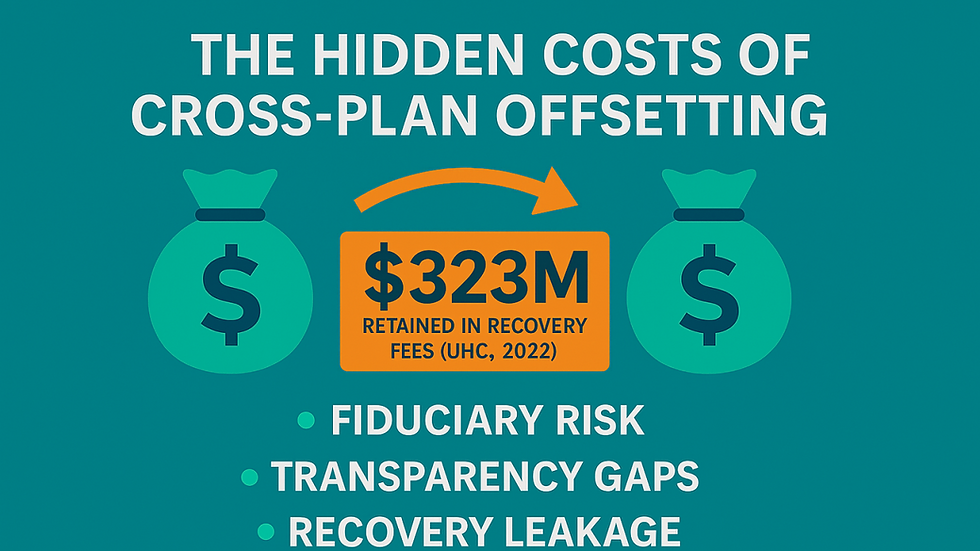
Post-Payment Conflicts – TPAs profiting from correcting their own errors.
OON Negotiations – Inflated out-of-network costs without meaningful caps.
Opaque Fees – Hidden charges and rebates that erode trust.
High-Dollar Claims – Large claims paid without proper independent review.
Subrogation & Recovery – Vendor-led recoveries that prioritize profit over plan savings.
Strengthening ASO Agreements
To protect participants, fiduciaries should negotiate stronger ASO provisions:
Data Ownership – Absolute plan ownership of claims data with penalties for late delivery.
Independent Post-Payment Review – Freedom to appoint an unbiased third party like ClaimInformatics.
OON Cost Controls – Enforce SPD caps (e.g., 1,000% of Medicare) with independent negotiators.
Fee Transparency – Full disclosure of all fees, capped recovery percentages, and penalties for non-disclosure.
High-Dollar Review – Independent review for all claims above $25,000 before payment.
Recovery Protections – Independent subrogation and recovery processes, free of TPA self-dealing.
SPD Recommendations: Protecting Participants
An SPD should clearly reflect these protections so participants know their plan is safeguarded:
Payments capped at 1,000% of Medicare.
Third-party review of high-cost claims.
Independent oversight of recoveries and subrogation.
Access to claims data within 10 business days.
Transparent and fair fees.
No hidden restrictions or gag clauses.
Why ClaimInformatics?
By outsourcing critical oversight functions to ClaimInformatics, fiduciaries gain:
Conflict-Free Oversight – No ties to TPAs or networks.
Audit-Ready Documentation – Defensible records for regulators.
Financial Impact – Proven recoveries and prevention of overpayments.
Ongoing Vigilance – Continuous monitoring for errors, abuse, and trends.
Take Action
Protect your plan, your participants, and your fiduciary standing—Partner with ClaimInformatics to strengthen ASO agreements and SPD protections. Please feel free to contact us at hello@claiminformatics.com to learn more. about our services


Comments