Restoring Fiduciary Trust in Healthcare: ClaimInformatics and Detego Health Redefine Independent Payment Integrity
- Dec 3, 2025
- 3 min read

Introduction
In the world of self-funded healthcare, trust is currency. Yet for many employers, that trust has eroded under a system where the same entities that administer claims also profit from “finding” savings within their own networks. This structural conflict leaves plan sponsors vulnerable to inefficiency, bias, and financial waste.
Until now!
ClaimInformatics and Detego Health have joined forces to fix that—rebuilding transparency, accountability, and fiduciary responsibility from the ground up.
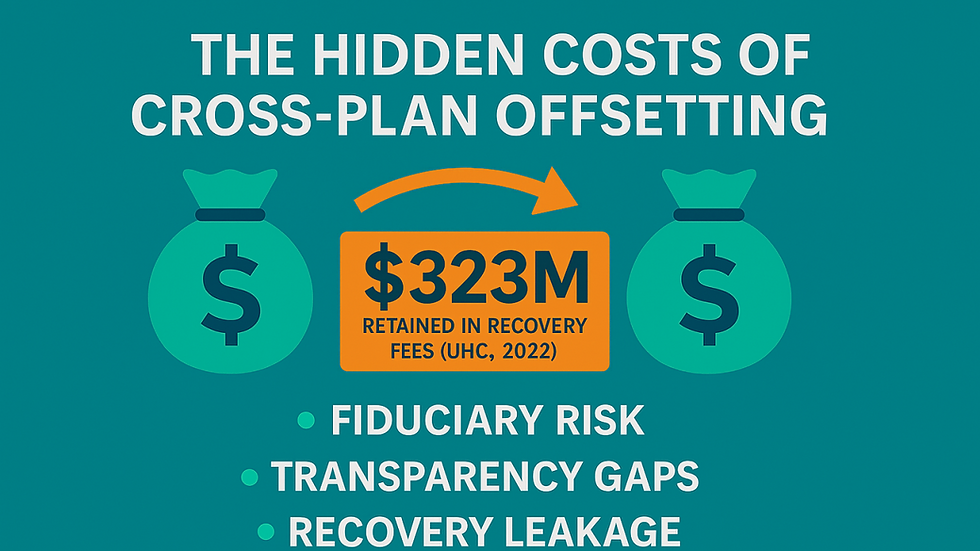
The Problem: Built-In Conflicts of Interest

Traditional third-party administrators (TPAs) often wear two hats: they manage the network, and they adjudicate claims. This dual role creates a clear conflict. When a TPA’s own contracted network is under review, how independent can that process truly be?
The result is a blurred line between oversight and operations, where the drive to preserve network relationships can outweigh the obligation to protect plan assets. For self-funded employers, the cost is tangible: millions of dollars are lost annually to miscoded, inflated, or fraudulent claims.
The Solution: True Independent Payment Integrity and Transparent Oversight
Through this strategic alliance, ClaimInformatics and Detego Health have created a blueprint for unbiased, pre-payment claim review.
Detego Health provides national network access and administrative infrastructure, while ClaimInformatics layers on a fully independent, evidence-based payment integrity platform. This “separation of powers” ensures claims are reviewed objectively, before payment is made, and without bias toward approval or network preservation.
“When your network administrator is also your claims gatekeeper, whose interests are really being protected?” — Stephen Carrabba, Co-Founder & CEO, ClaimInformatics
How It Works
The integrated solution delivers independence at scale, serving over 100,000 covered lives across the nation. The platform brings together:
Clinical and Coding Intelligence: CMS-aligned edits, NCCI rules, SPD-based validations, and advanced AI-Driven FWA detection models.
Pre-Payment Protection: Applies the payment policy and coding errors and medically unlikely scenarios before payment.
ERISA & Plan Document Alignment: Ensures fiduciary compliance by validating claims against plan documents and documenting the rationale for every decision.
Provider Relationship Preservation: Reduces friction by ensuring accurate, policy-consistent payments for the first time.
“ClaimInformatics brings institutional-quality payment integrity that our employer groups need—transparent, evidence-based, and completely independent from our network operations.” — Alan Wilson, President & CLO, Detego Health.
Fiduciary Framing with Quantitative Proof
This ERISA-driven strategy ensures prudence in fiduciary oversight, proper administration of plan assets, monitoring of service providers, and adherence to plan documents.
Self-funded employers using this approach experience:
2–8% reduction in inappropriate medical spend (vs. 1–3% post-payment recovery)
Lower administrative burden, with fewer disputes and audits
Enhanced DOL audit readiness through transparent documentation
Faster payments for compliant providers
This model not only safeguards plan assets but also improves member experience and provider trust across the ecosystem.

Why It Matters
The healthcare market is demanding change. CFOs and benefits leaders recognize the risks inherent in bundled TPA models. They want network access without network bias, payment integrity without competing incentives, and fiduciary oversight that stands up to scrutiny.
With this partnership, ClaimInformatics and Detego Health are setting up a new industry benchmark for how fiduciary accountability should look in healthcare claims administration.
About the Partners
ClaimInformatics is a healthcare analytics and payment integrity firm specializing in pre-payment and post-payment review, combining AI-driven FWA detection with clinical rule logic to ensure every claim is paid accurately, transparently, and compliantly. Learn more: www.claiminformatics.com
Detego Health® is a national Third-Party Administrator (TPA) offering transparent, data-driven plan administration and reporting for self-funded and level-funded employers. Learn more: www.detegohealth.com


Comments