Systematic Overbilling and Upcoding at Women’s Health Care Group - What Self-Funded Plans Should Know
- Sep 23, 2025
- 2 min read
Introduction
A recent investigation into Florida Woman Care — one of the largest women’s health providers in the state — revealed troubling allegations of systematic overbilling and upcoding designed to pad private equity profits. These practices come at a steep cost to patients and health plans.

As highlighted in NBC News’ Cost of Denial series, this is not an isolated case. While Florida Woman Care is under investigation, the truth is that upcoding, hidden fees, and billing for services not rendered are pervasive across the healthcare system. These aren’t rare outliers—they are standard tactics embedded in the playbooks of revenue cycle companies nationwide.
At ClaimInformatics, we see these abuses every single day in our reviews of self-funded plans. It’s why independent oversight isn’t optional—it’s a fiduciary responsibility. Without proactive monitoring, plan sponsors risk unknowingly subsidizing inflated charges that put both members and plan assets at risk.
Key Systematic Overbilling and Upcoding Allegations
Upcoding & Hidden Fees: Providers tied to Florida Woman Care allegedly used billing codes to inflate reimbursement and disguise administrative overhead, driving up patient and plan costs.
Lack of Disclosure: Neither patients nor health plans were informed about these administrative charges buried in claims, which undermines informed decision-making.
Profits Over Patients: Overbilling enriched private equity owners of women’s health providers—pitting shareholder profits against fiduciary duty to plan members.
Why Self-Funded Plans Are Particularly Vulnerable
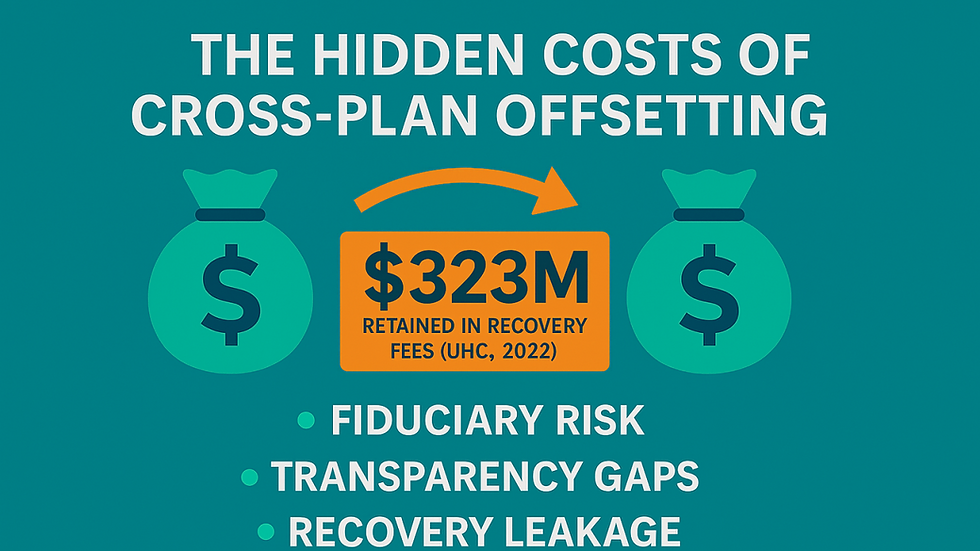
Fiduciary Exposure: Under ERISA, sponsors must act prudently and solely in participants’ interests. Paying inflated or hidden fees can be a breach of duty.
Opaque Contracts: Without clear terms and ongoing monitoring, it’s nearly impossible to spot disguised charges.
Cost-Sharing Harm: Members with high deductibles and co-pays bear the brunt of inflated claim costs.
What Fiduciaries Should Do Now
Review Claims for Upcoding & Overhead: Require independent reviews of claims to separate legitimate clinical services from padded or administrative charges.
Demand Full Transparency: Ensure vendors and providers disclose all fees—no hidden codes, no surprises.
Protect Through Contracts: Add clauses that prohibit hidden fees and mandate disclosure before new codes are used.
Engage Independent Oversight: Work with specialists like ClaimInformatics to monitor claims pre- and post-pay, ensuring payments reflect only necessary, reasonable care.
Bottom Line
This investigation shines a light on how healthcare billing practices are routinely exploited for profit—with patients and plan sponsors footing the bill.
For fiduciaries of self-funded plans, the takeaway is clear:
Don’t wait for headlines.
Don’t assume your vendors are protecting you.
Proactively engage independent oversight.
At ClaimInformatics, we see these billing abuses every day—and we stop them before they drain plan assets and increase member liability.
Transparency, oversight, and accountability aren’t optional. They are fiduciary obligations.


Comments