The 401(k) Lesson: Why Compliance Matters in Self-Funded Healthcare
- Sep 30, 2025
- 3 min read

Introduction - The rise of fiduciary lawsuits
The rise of fiduciary lawsuits permanently changed the 401(k) industry. Employers learned that failing to monitor vendors, fees, and governance structures could lead to costly litigation and reputational damage.
Today, self-funded health plans are entering that same era of scrutiny. Just as 401(k) plan sponsors had to adapt to fiduciary standards, employers offering self-funded healthcare must now comply with ERISA and new mandates under the Consolidated Appropriations Act (CAA 2021). Those who fail to evolve risk legal action, regulatory enforcement, and financial harm to both the plan and its participants.
The 401(k) Compliance Era: A Hard Lesson
Compliance wasn’t voluntary for retirement plan sponsors — lawsuits and Department of Labor enforcement made it mandatory. Three landmark cases reshaped governance expectations:
Tussey v. ABB (2012): Employers held liable for failing to monitor service providers and recordkeeping fees.
Tibble v. Edison (2015): The Supreme Court established the ongoing duty to monitor investments.
Cassell v. Vanderbilt (2021): Emphasized the necessity of prudent vendor management.
Together, these rulings established a governance framework in which transparency, benchmarking, and fiduciary diligence became non-negotiable.
Why Self-Funded Healthcare Is Next
The same compliance pressures that transformed 401(k) plans are now converging on health plans:
Litigation is rising: Employers, including Johnson & Johnson and Kraft Heinz, have been sued for failures in PBM pricing oversight and vendor management.
CAA 2021 mandates disclosure: Plans must ensure transparent broker compensation, Rx cost reporting, and access to claims data.
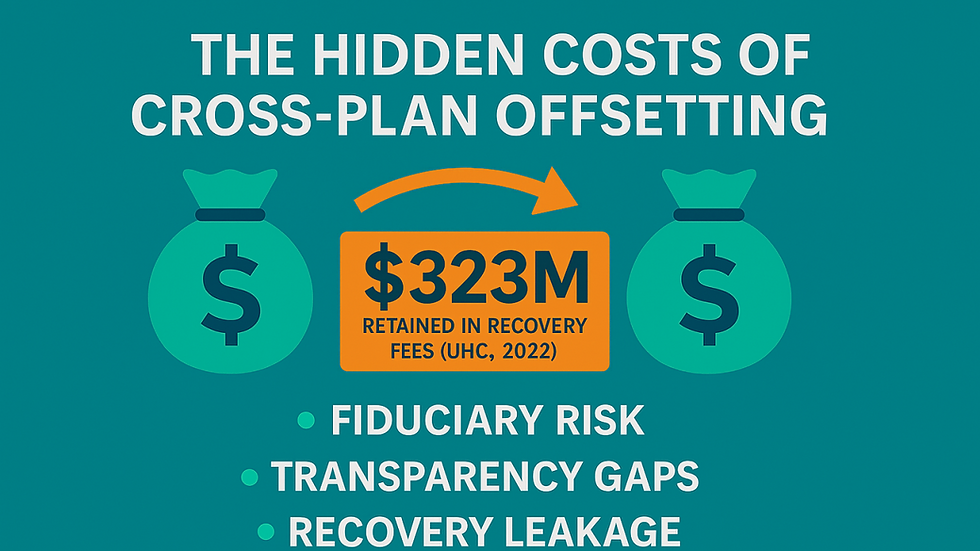
Hidden costs remain pervasive: PBMs and TPAs often retain rebates, apply spread pricing, or draft opaque contracts that inflate costs.
With the greater transparency mandated by the CAA comes greater responsibility. Plan fiduciaries can no longer claim ignorance; they must act prudently on the data they receive. At the same time, governmental oversight, particularly from the Employee Benefits Security Administration (EBSA), is intensifying, reinforcing that failures in compliance will trigger not only lawsuits but also regulatory action.
Simply put, self-funded health plans are the new frontier of fiduciary accountability.
Compliance Red Flags in Self-Funded Plans
Employers should view the following as clear warning signs that fiduciary obligations may already be compromised:
1. No access to claims or pricing data.
2. Lack of disclosure around broker or consultant compensation.
3. PBM or TPA agreements without unrestricted audit or oversight rights.
4. Vendor fees that haven’t been independently benchmarked in years.
5. Absence of a formal fiduciary committee or governance documentation.
These deficiencies mirror the exact lapses that fueled the wave of 401(k) lawsuits — and they are now surfacing in health plan litigation.
What Employers With Self-Funded Plans Must Do Now To Ensure Compliance
To avoid becoming the next compliance headline, employers must apply the same level of rigor to health plans that retirement plans adopted years ago:
Demand transparency from brokers, consultants, TPAs, and PBMs.
Benchmark vendor fees regularly against independent market data.
Establish a fiduciary committee with a formal charter and defined responsibilities.
Protect plan assets with prudent oversight and internal controls.
Monitor service providers for performance, accountability, and conflicts of interest.
Document all governance decisions and vendor oversight processes.
Educate fiduciaries on ERISA obligations and new CAA compliance requirements.
The Lessons from 401(k) experiences
The 401(k) experience reveals a simple truth: ignoring fiduciary responsibilities leads to lawsuits, personal liability, regulatory action, and costly settlements. 401(k) oversight is here for health plans. The same standards of diligence, transparency, and prudent governance that reshaped retirement plans are now unavoidable in healthcare.
With the CAA’s transparency mandates and EBSA’s heightened oversight, compliance is no longer optional — it is essential. Employers who act now will strengthen governance, reduce legal risk, lower costs, and build trust with employees. Those who delay may find themselves reliving the painful wave of 401(k) litigation — only this time, in the realm of healthcare.
Claiminformatics Uses Payment Integrity to Deliver Fiduciary Compliance For Self-Funded Plans
ClaimInformatics partners with employers to uncover hidden fees, monitor service providers, ensure compliance, and build defensible fiduciary processes. Contact us today to safeguard you and your self-funded health plan.


Comments