Payment Integrity or Revenue Protection?
- Oct 2, 2025
- 2 min read
What Plan Sponsors Need to Know About HCSC’s Direct to Client Program

Introduction
“Plan sponsors are being charged to fix mistakes they already paid to avoid. That’s not payment integrity—it’s revenue protection disguised as oversight.” Stephen Carrabba, Founder/CEO Claiminformatics
This quote captures the frustration many self-funded plan sponsors are facing. At ClaimInformatics, we’ve been tracking a troubling trend: carriers creating barriers for plan sponsors who want to exercise independent fiduciary oversight.
According to Chris Deacon, the HCSC “Direct to Client” Program, Health Care Service Corporation (HCSC), one of the largest Blue Cross Blue Shield Association franchisees, is launching a new “Direct to Client (DTC)” program. On paper, it’s positioned as a payment integrity initiative. In practice, it’s a pay-to-fix-what-you-already-paid-for loop.
“Readers' digest version: if you try to bring in your own oversight, you’ll either face enough friction to give up—or pay steeply for the privilege. Whether the intent is deterrence, revenue extraction, or both, the result is the same.” Chris Deacon
Here’s How Their Payment Integrity It Works
Plan sponsors don’t get to choose between HCSC’s internal Advanced Payment Review (APR) and the DTC Program. They must pay for both.
The price tag is steep: $861 per case reviewed and $2,638 per pre-pay flag request. For large employers, those costs add up fast.
Plan sponsors’ chosen payment integrity vendors are restricted in scope. Medical necessity reviews and pre-payment independent reviews are currently off the table at HCSC.
Reporting, communication, and escalation? All controlled by HCSC—not the plan sponsor or their fiduciary partners.
The Fiduciary Problem
ERISA requires plan fiduciaries to act prudently and solely in the interest of plan participants. But under DTC, fiduciaries are forced to:
Pay the carrier to process claims correctly the first time,
Pay again for a third-party vendor to catch their payment errors, and
Pay a third time for HCSC to “approve” or oversee the very vendor whose involvement is necessary only because of carrier errors.
That isn’t oversight — it’s abusive revenue extraction. And why does it happen? Because they could — until now.
Why This Matters for Plan Sponsors
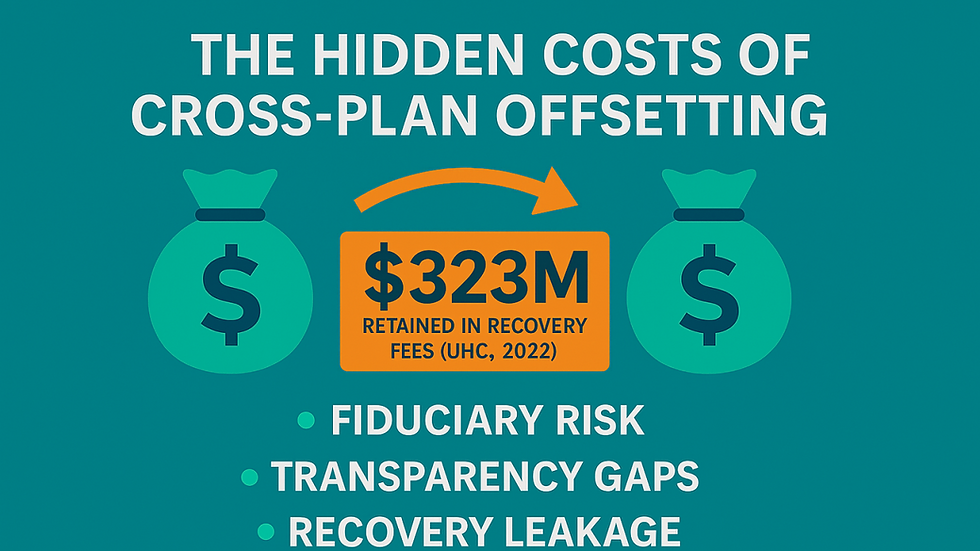
Fiduciary Exposure: Paying carriers multiple times to fix their own mistakes raises questions of prudence and reasonableness.
Cost Containment: Excessive fees cut directly into plan assets—employer dollars and participant contributions.
Control and Transparency: By limiting vendor authority and requiring all communications to flow through the carrier, HCSC keeps employers in the dark.
The ClaimInformatics Perspective
At ClaimInformatics, we believe plan sponsors should not have to pay three times for claim accuracy. Independent oversight should be:
Transparent
Unrestricted by carrier gatekeeping
Focused on fiduciary compliance, not revenue protection
Plan sponsors deserve a system where errors are prevented, not monetized.
Conclusion
As renewal season approaches, fiduciaries should carefully review contract terms and challenge “mandatory” payment integrity programs that shift costs back onto plans. If you’re being asked to pay to fix what you’ve already paid for, the time to push back is NOW!


Comments