Aetna & Optum Settle “Dummy Codes” Case for $8.4M: What Fiduciaries Should Learn.
- Sep 19, 2025
- 2 min read

After nearly a decade of litigation, Aetna Life Insurance Company and OptumHealth Care Solutions have agreed to pay $8.4 million to settle allegations that they concealed administrative fees inside claims using so-called “dummy codes.”
🚩 Allegations
Plaintiff Sandra Peters argued that Aetna and Optum:
Directed providers to submit claims with “Administrative Add-On Services.”
Masked Optum’s administrative fees as medical expenses, raising member cost-sharing.
Failed to disclose these hidden charges to plan members or sponsors, violating ERISA fiduciary duties.
🏛️ Litigation Timeline
2019: Case dismissed by the district court.
2021: Fourth Circuit revived claims, finding plausible evidence of disguised fees.
(Peters v. Aetna Inc., No. 19-2085, Opinion PDF).
2022: Supreme Court denied review.
2025: Case settled ahead of trial.
“Neither Aetna nor Optum disclosed to members that they would be charged for Optum’s administrative fees, nor that such charges would increase the members’ cost-sharing obligations.”
$8.4M total: $4.6M from Aetna, $200k from Optum, $3.6M to attorneys’ fees.
Class: Over 250,000 members who paid cost-sharing on claims with “Administrative Add-On Services.”
Distribution: Pro-rata payments based on overcharges.
“Class Members are those who, during the Class Period, paid cost-sharing amounts on claims that included Administrative Add-On Services submitted by providers contracted through Optum.”
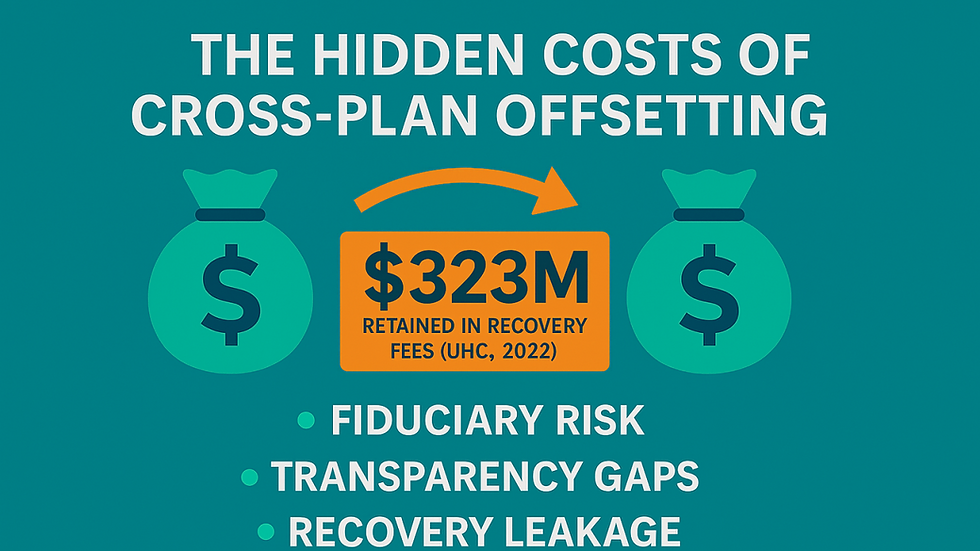
🔍 Broader Implications for Self-Funded Plans
Transparency in Billing – Overhead can be hidden in coding, obscuring true medical costs.
ERISA Fiduciary Duties – Courts reaffirm that insurers and vendors may both be fiduciaries when they impact plan assets.
Vendor Oversight – Insurer–vendor relationships blur responsibilities; fiduciaries must demand clarity.
Access to Data – Without full access to your claims and payment data, you cannot identify these hidden costs, conflicts, and fiduciary risks.
Individual Action, Systemic Change – One participant’s complaint yielded relief for 250,000 people, showing the power of ERISA enforcement.
✅ The Fiduciary Takeaway
For self-funded sponsors, the message is clear:
Scrutinize claims for hidden charges.
Review vendor arrangements to uncover disguised costs.
Document oversight to prove prudent process.
At ClaimInformatics, we help fiduciaries shine a light on opaque billing practices and protect plan assets from disguised fees. Transparency isn’t optional — it’s your duty.


Comments