ERISA-Covered Companies Must Disclose Health Plan Costs
- WixBuddy Plus

- Jun 25, 2025
- 8 min read
Starting in 2022, an estimated 2.5 million employer-sponsors of health plans are required to adopt new fee and pricing transparencies due to amendments made to ERISA. While ERISA has focused on retirement service fees in the past, the spotlight is now on healthcare costs.
The requirements fall under the Affordable Care Act (ACA) and Consolidated Appropriations Act, 2021 (CAA 2021), and affect organizations covered by the Employment Retirement Income Security Act of 1974 (ERISA).
ERISA applies to most private companies that offer healthcare and retirement plans to employees. Complying with ERISA fiduciary duties for group health plans has been challenging due to the lack of fee transparency in the industry. However, the new transparency rules put more fee and pricing information into the hands of health plan fiduciaries and other stakeholders to shed light on these fees.
The new transparency rules put more fee and pricing information into the hands of health plan fiduciaries and other stakeholders to shed light on these fees.
An array of required disclosures
These rules place new transparency obligations on group health plans and health insurance issuers subject to ERISA, including:
Publicly reporting health plan prices for medical and prescription drug services,
Developing cost-sharing tools for plan participants,
Eliminating surprise billing,
Removing gag clauses from health plan contracts, and
Reporting healthcare, pharmacy benefits, and prescription drug costs to the federal government.
Annually, starting in 2022, employer-sponsors of group health plans will be required to submit attestations to group health plan regulators that they have removed gag clauses in health plan contracts. Under CCA 2021, brokers and consultants are required to disclose fees to health plan fiduciaries so the fiduciaries can attest to their reasonableness.
The new transparency rules also require brokers and consultants, who provide services to group health plans, to provide fee disclosures to plan fiduciaries. Without knowing how much they are paying, plan fiduciaries cannot satisfy their ERISA obligations to determine the reasonableness of fees.
ERISA fiduciary duties
When advising clients, in-house counsel should know their organization’s disclosure obligations and how they affect the fiduciary obligations of employer-sponsored group health plans. While many of these new transparency obligations can be delegated to third parties, group health plan fiduciaries remain responsible for monitoring fiduciary delegations and determining that group health plan fees are reasonable.
Fiduciary status is based on the functions performed for, or on behalf of, the plan, and include committees or individuals that oversee employee benefits and administer the group health plan. Fiduciaries of ERISA plans are required to administer the plan in accordance with ERISA’s fiduciary duties.
Strict obligations
Many private employer-sponsored group health plans are subject to ERISA, which places strict obligations on the conduct of plan fiduciaries. ERISA requires them to act solely in the interest of plan participants and beneficiaries with duty of care, skill, diligence, and prudence. This includes defraying reasonable expenses of administering the plan.
When advising clients, in-house counsel should know their organization’s disclosure obligations and how they affect the fiduciary obligations of employer-sponsored group health plans.
ERISA’s prohibited transaction rules limits certain plan transactions with “parties in interest,” which include insurers and service providers to the plan. The service provider exemption permits a plan to pay reasonable compensation to a party providing necessary services for the plan. Therefore, fiduciaries of ERISA group health plans have a duty to ensure that the assets of the plan, including participant contributions, are used only to pay benefits or the plan’s reasonable expenses.
Avoiding lawsuits
While ERISA applies equally to retirement and health and welfare plans, the fiduciary spotlight has traditionally been focused on retirement plans, which have been subject to a dramatic increase in class action fee litigation resulting in high-dollar settlements. As a result, retirement plan fiduciaries have been motivated to develop rigorous plan governance and oversight of service providers. Historically, less attention has been paid to good ERISA hygiene for group health plans, but the new transparency rules necessitate a fresh review of group health plan fiduciary governance and administration.
Broker and consultant compensation disclosures
Failure by the broker or consultant to comply with the broker-consultant disclosure requirements means the service arrangement is not reasonable. And, therefore, it is a prohibited transaction. Specifically, the CAA 2021 created disclosure requirements under Section 408(b)(2) of ERISA that apply to brokers and consultants providing services to group health plans by codifying rules similar to the ERISA retirement plan disclosure regulations. ERISA section 408(b)(2) exemption provides a statutory exemption for reasonable contracts with service providers if the services are necessary for operation of the plan and no more than reasonable compensation is paid for the services.
The new rules apply to any service provider who reasonably expects to receive US$1,000 (adjusted for inflation) or more in direct or indirect compensation for:
Brokerage services provided to an ERISA-covered group health plan with respect to the selection of health insurance products (including vision and dental), recordkeeping services, medical management vendor, benefits administration, stop-loss insurance, pharmacy benefit management services, wellness services, transparency tools and vendors, group purchasing organization preferred vendor panels, disease management vendors and products, compliance services, employee assistance programs, or third-party administration services, or
Consulting services related to the development or implementation of plan design, insurance selection (including vision and dental), recordkeeping, medical management, benefits administration selection, stop-loss insurance, pharmacy benefit management services, wellness design and management services, transparency tools, group purchasing organization agreements and services, participation in and services from preferred vendor panels, disease management, compliance services, employee assistance programs, or third-party administration services for an ERISA-covered group health plan.
The US$1,000 compensation threshold includes amounts paid to a service provider’s affiliate or subcontractor. Note that this threshold is much lower than the US$5,000 threshold required on Schedule C of the DOL’s Form 5500. The term “compensation” includes both cash and non-monetary compensation valued at more than US$250 (adjusted for inflation) paid, in the aggregate, during the term of the arrangement.
The fiduciary spotlight has traditionally been focused on retirement plans, which have been subject to a dramatic increase in class action fee litigation resulting in high-dollar settlements.
Like the disclosure rules applicable to retirement plan service providers, these rules require a health plan service provider to disclose, in writing, the following information to the group health plan fiduciary:
A description of the services to be provided to the covered plan pursuant to the contract or arrangement;
If applicable, a statement that the service provider (or an affiliate or subcontractor) will provide, or reasonably expects to provide, fiduciary services to the covered plan;
A description of all direct compensation the service provider (or an affiliate or subcontractor) reasonably expects to receive in connection with the provision of services;
A description of all indirect compensation the service provider (or an affiliate or subcontractor) reasonably expects to receive in connection with the provision of services (including incentives paid to a brokerage firm not solely related to the contract with the covered plan), a description of the arrangement between the payer of the indirect compensation and the recipient service provider, a description of the services for which the indirect compensation is received, and the identity of the payer of the indirect compensation;
To the extent compensation is paid among a service provider, the service provider’s affiliate, or the service provider’s subcontractor on a transaction basis (such as commissions or finder’s fees), a description of any such arrangement and identification of the payers and recipients of such compensation (including the status of a payer or recipient as an affiliate or a subcontractor);
A description of any compensation that the service provider (or an affiliate or subcontractor) reasonably expects to receive in connection with termination of the contract or arrangement, and how any prepaid amounts will be calculated and refunded upon such termination; and
A description of the way any direct or indirect compensation will be received by the service provider (or an affiliate or subcontractor).
This information must be disclosed to the responsible plan fiduciary before the contract or arrangement is established, extended, or renewed. In addition, the service provider has an affirmative obligation to notify the plan fiduciary of any change to the above required disclosures as soon as practical, but generally not later than 60 days from the date the service provider is informed of the change. The service provider must also provide other compensation information requested by the plan fiduciary for the plan to comply with its annual Form 5500 reporting and disclosure requirements.
A plan fiduciary could be in breach of their fiduciary duty if they fail to obtain these disclosures. Without disclosures, it is impossible to determine the reasonableness of service provider compensation or evaluate potential conflicts of interest.
The new disclosure rules place increased obligations on health plan fiduciaries to determine whether any direct or indirect compensation paid to a broker or consultant in connection with an ERISA group health plan is reasonable.
If the disclosures provided by the service provider turn out to be incomplete or inaccurate, a health plan fiduciary could still satisfy the prohibited transaction exemption if they relied in good faith on a service provider’s disclosures. In such a case, the plan fiduciary must take reasonable steps to obtain the missing or incorrect information upon discovery, inform the DOL, and consider whether to terminate or continue the arrangement if the service provider fails to comply with a request for information within 90 days. In a bulletin issued in late 2021, the DOL indicated that it will not issue further guidance on the CAA 2021 broker/consultant disclosure rules and encouraged plan fiduciaries to refer to the existing retirement plan disclosure rules for additional guidance.
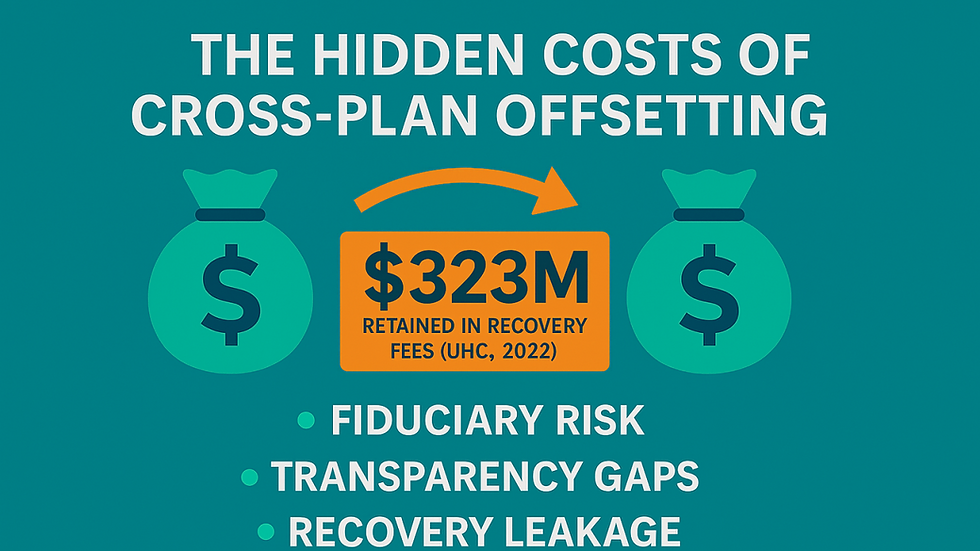
The new disclosure rules place increased obligations on health plan fiduciaries to determine whether any direct or indirect compensation paid to a broker or consultant in connection with an ERISA group health plan is reasonable. There are penalties for failure to comply with these new disclosure requirements. They could include the plan fiduciary being held liable for any losses to the plan that result from the prohibited services arrangement, including restoration to the plan of any excess fees or commissions, service provider liability for knowing participation in a prohibited transaction, and DOL actions or settlements.
7 fiduciary best practices for group health plans
Plan sponsors — the employer or organization that establishes the employee benefit plan — should assess the hygiene of their group health plan governance and fiduciary oversight of service providers. Plan sponsors should engage in the following action items:
Consider whether to formally delegate fiduciary responsibility for group health plan governance to a committee and develop a committee charter to set forth committee responsibilities and any limitations on authority.
Confirm group health plan fiduciaries are covered under existing fiduciary liability insurance and indemnified in plan documents.
Review existing group health plan service provider agreements to confirm if the new broker/consultant disclosure requirements apply, and if so, request service provider fee disclosures.
Evaluate service provider disclosures in accordance with the ERISA fiduciary requirements in relation to the quality, nature, and scope of the services. Consider following existing DOL guidance on retirement plan fees. Another helpful resource is the DOL white paper, “Understanding your Fiduciary Responsibilities under a Group Health Plan.”
Consider amending service provider agreements to incorporate contractual obligations requiring the service provider to cooperate with the plan sponsor in meeting the new group health plan transparency and fee disclosure requirements.
Establish a process to regularly monitor group health plan fees to ensure that they are reasonable and in accordance with industry standards. Consider conducting an RFP for group health plan service providers every few years to benchmark fees.
Document the review process and specify how the reasonableness of compensation was determined in selecting and monitoring service providers.
Plan sponsors — the employer or organization that establishes the employee benefit plan — should assess the hygiene of their group health plan governance and fiduciary oversight of service providers.
Documentation of a well-designed and prudent fiduciary process for group health plan benefit plan governance is key. By addressing best practices, effective plan governance and fiduciary obligations proactively, plan sponsors and fiduciaries of group health plans will be better positioned to defend against government audits and excessive fee litigation.


Het is belangrijk dat bedrijven die onder ERISA vallen, transparant zijn over de kosten van hun zorgplannen om werknemers goed te informeren. Dynabet Casino https://dynabet-casino.nl biedt een breed scala aan spannende spellen en aantrekkelijke bonussen, waardoor het een favoriete keuze is voor spelers in Nederland. Bovendien zorgt hun gebruiksvriendelijke interface ervoor dat zowel nieuwe als ervaren spelers eenvoudig kunnen genieten van het spelaanbod.